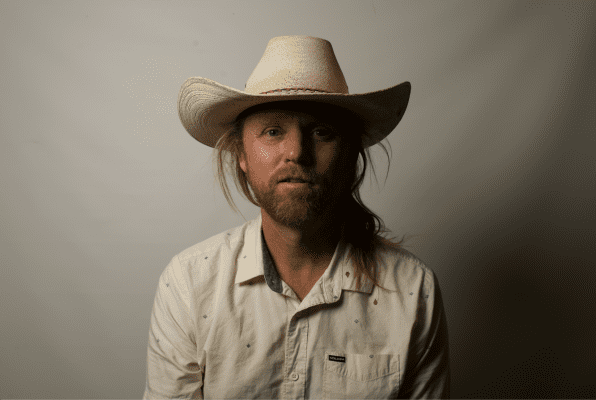
Jacobus “Jacoby” Vandervlis, 55, celebrated his first birthday last month.
That’s what he calls it.
Last year, on Aug. 3, Vandervlis was rushed to the hospital when flu-like symptoms developed into a full-body breakdown and mental stupor. His mother, Helena, 82, had found him on the floor of their shared house in Hermosa Beach in a pool of blood. The robust, 6-foot-7, 250-pound construction worker had fallen.
Five weeks later, after being shuffled among neurologists and put temporarily into a medically induced coma, he was released. But the battle was far from over.
Vandervlis had contracted West Nile virus from a mosquito bite on his foot in late July. He was in bed in his Hermosa Beach home when he heard a buzzing around his head.
“I pulled the sheets way over my head,” he said. “But I’m 6-foot-7, and my feet stick out of the bed.”
It took weeks for doctors to determine what was wrong. His final diagnosis included West Nile virus encephalitis (inflammation of the lining surrounding the brain), myelitis (inflammation of the spinal cord) and brachial neuritis (a nerve disorder affecting the shoulders and arms).
Vandervils was lucky to be alive, the doctors said, even if he didn’t much feel that way.
“They wanted to release me on Friday, Sept. 13,” Vandervlis recalled. “I said no. I had had enough of 13 and of 2013.”
He was released into his mother’s care on the 12th and went home virtually paralyzed, in diapers, with a catheter, unable to wash or feed himself and 100 pounds lighter than he had been five weeks before.
11 years of West Nile
West Nile virus is an arthropod-borne virus (arbovirus) most commonly spread by infected mosquitoes. According to the U.S. Department of the Interior and the U.S. Centers for Disease Control and Prevention, since West Nile virus was first isolated in 1937, it was known to cause asymptomatic infection and fevers in humans in Africa, West Asia and the Middle East.
Human and animal infections were not documented in the Western Hemisphere until the 1999 outbreak in the New York City metropolitan area. Since then, the disease has spread across the United States. In 2003, West Nile was found in 46 states and caused illness in more than 9,800 people.
The first reported human infections of West Nile in Los Angeles County occurred in 2003. In 2004, there were 306 confirmed cases, according to the California Department of Public Health. The incidence of human infections in the county has fluctuated over the past decade: 2004 remains the highest, to date, and 2010 saw the lowest rate, with four cases. However, 2012 and 2013 saw a resurgence in human incidence of the virus.
On July 3, Dr. Laurene Mascola, chief of the Acute Communicable Disease Control Program at the Los Angeles County Department of Public Health, issued a public letter to guide physicians and laboratory directors through this year’s West Nile virus season, which typically runs from May to November.
“The 2014 West Nile virus season in Los Angeles County follows on the footsteps of the second and third highest counts of human infection in 2012 and 2013, respectively,” the letter reads. “WNV has already started this year with the detection of a WNV positive chicken at the beginning of January in the San Fernando Valley area. Other environmental indicators including WNV positive dead birds and mosquito pools have been detected near the South Bay area.”
According to the Department of Public Health, as of Oct. 2, the county has seen 90 cases of West Nile in humans this year. Sixty-six patients have been hospitalized, and three have died. Just three of the county’s West Nile patients this year have been identified within Service Planning Area (SPA) 8, the South Bay. Last year, 28 were infected here.
Dr. Lisa M. Santora is the chief medical officer for Beach Cities Health District in Redondo Beach. She joined BCHD, the nation’s largest preventive health agency, in 2008 to provide oversight for evidence-based community strategies to improve the health and well-being of Beach Cities residents.
She also has unique experience with West Nile: She encountered the virus during her 2002 medical residency in Erie County, N.Y., just three years after it hit the United States. Her subsequent public health training also included vector research of mosquitoes.
“Most people consider West Nile virus as associated with humans because, of course, we’re humans,” said Santora. “But we are considered a dead-end host. Birds are the primary host of the virus.”
The sentinel event, or the signal that the virus is present in a community, she said, is the identification of infected dead birds.
“The virus cannot survive in us like it can survive in birds,” Santora said. “It’s important to take precaution and make the right decisions, but it’s only the one in five of us (who get the virus) that will present any symptoms.”
Santora said that 80 percent of people who are infected will never know they have West Nile. Of the 20 percent who exhibit symptoms, usually only 1 percent develop the encephalitis or meningitis associated with death. The remaining 19 percent will experience flu-like symptoms. People over the age of 50 and those who are immunocompromised have the highest rates of complications from the virus.
“Meningitis and encephalitis are your biggest concerns because there is no treatment for it,” Santora said. “When you have an illness like these, it can take 12 weeks or more until you start to rebound … a quarter of a year until the symptoms really truly start to subside. It’s not just once a person gets discharged from a hospital, it’s done … the recuperation from a brain injury is huge.”
Preventive measures
Medical professionals such as Santora urge South Bay residents to remember that prevention is paramount.
“First, know that there are public health departments starting from the CDC down to the California Department of Public Health down to our Los Angeles County Department of Public Health that are all working in concert to address the seasonal epidemic,” Santora said. “There are resources readily available to (residents) at all of those locations to see about the current status of the epidemic in their community.”
In terms of mosquito-bite prevention, Santora echoes the advice put out by organizations like the CDC: use DEET-based insect repellant, be especially careful at dawn and dusk, and drain any standing water. Go to www.24hpestpros.com to find more info.
“In our community a lot of people are concerned about the use of DEET,” she said. “But the EPA just released in 2014 … an update to their safety profile of DEET. … There is no research to show that there is any adverse effect on their health, and protecting yourself from a bite is really important.”
Santora urges anyone with concerns about the use of DEET to visit the EPA’s website and review the new safety profile.
The second precaution, Santora said, is more difficult for the Beach Cities Health District to navigate. Part of the BCHD’s main philosophy for preventive health care is physical activity, and she knows many residents want to exercise outdoors at the beginning or end of the day.
Santora recommends extra diligence with insect repellant during those hours and being mindful about where you choose to exercise.
Finally, standing water is an ideal breeding ground for mosquitoes.
“With the heat we’ve had, we have to make sure we are draining baby pools and any other standing water,” she said. “You don’t want to create a breeding ground yourself. Diseases like West Nile virus thrive in heat, especially above 86 degrees.”
The best weapon to fight the virus, like virtually any disease, she says, is having a healthy immune system.
“From the health district perspective, we invest in physical activity and healthy behaviors because diseases like diabetes and heart failure are immunocompromising,” Santora said. “We really try to prevent those chronic diseases because the 50-year-old with diabetes is going to be a lot higher risk than the 50-year-old who is physically active and healthy.”
Vandervlis’ recovery

Vandervlis has recently been able to stop using his walker. He remains on a cocktail of pharmaceuticals, including Keppra, an anti-seizure medication to help reduce inflammation in the brain, and pain medications. The pain, largely in his shoulders and neck, hasn’t subsided, and he finds it hard to get much done. His work disability is permanent.
“I’ve had to grieve over it,” Vandervlis said. “I came back from all of this half the man that I was. I’ll never be able to go back to work. I still have little strength or motor skills – I have trouble opening a Ziplock bag.”
The past year has been hard on his mother, Helena, too. She sat in the hospital, day after day, with her son until he finally begged her to go home. When Vandervlis was released, another challenge began.
“It was like having a baby again when he came home,” she said. “I’m 82 years old. I couldn’t do it myself.”
Helena was also frustrated by the number of doctors Vandervlis was shuffled between and said he was treated as “taboo.”
Helena and Vandervlis said they found the best help in a neurologist in Inglewood, Dr. David Kheradyar. They also hired a nurse, Cindy, to help at home.
Between those caregivers and a constant rotation of physical, emotional and occupational therapy, Vandervlis is beginning to come around.
Vandervlis does identify one silver lining about his illness: The experience helped him reconnect with a son he hadn’t seen in 30 years. He said he realized it was time to start making amends.
“People ask if I saw the light or something when I was in the coma,” Vandervlis said. “No. All it was was a long nap, and I woke up and said, ‘Holy crap, what happened to me?’
“I’ll never be normal,” he said. “But I am happy to be above ground. I’m starting over in life again.”
This story originally appeared in the Easy Reader on October 9, 2014.